Manual Dexterity
It has been called “the bible of psychiatry,” the guidebook used by mental health professionals throughout the United States to diagnose mental illness, which is the first step is selecting a treatment. Published by the American Psychiatric Association, the Diagnostic and Statistical Manual of Mental Disorders contains detailed descriptions of a wide variety of behavioral maladies. It is used not only by psychiatrists, psychologists, social workers, and other therapists, but also by insurance companies, to determine coverage for mental health treatment, and school districts, to provide funds for special services for students with developmental problems.
Professor Emeritus Robert Spitzer, MD, is widely considered to be the “grandfather” of the DSM, transforming the manual in 1980 from a list of diagnostic codes and brief definitions into a scientifically based compendium of operationalized diagnostic criteria that allowed mental health professionals to reliably make psychiatric diagnoses. The DSM has been revised several times since to reflect new information gleaned from psychiatric research. A number of P&S and New York State Psychiatric Institute faculty members worked on earlier editions of the manual, and the most recent—DSM-5, published in May 2013—is no exception.
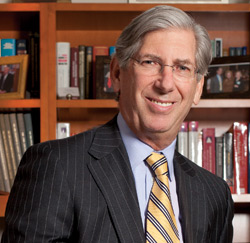 Jeffrey Lieberman, MD. Photo by Jörg Meyer
Jeffrey Lieberman, MD. Photo by Jörg MeyerJeffrey Lieberman, MD, professor and chair of psychiatry at P&S and director of NYSPI, began his term as president of the APA just as the new edition was going to press and helped to orchestrate its launch. Several faculty joined the work groups involved in making changes to DSM-5, and two of them served as work group chairs: David Shaffer, MD, professor of psychiatry and of pediatrics, headed the ADHD and disruptive behaviors work group, and B. Timothy Walsh, MD, professor of pediatric psychopharmacology, led the eating disorders work group.
P&S alumni also contributed to DSM-5, including Kimberly Ann Yonkers’86, professor of psychiatry and of obstetrics, gynecology, and reproductive sciences at Yale, who served on the task force that coordinated the efforts of all the work groups. Arthur J. Barsky’69, professor of psychiatry at Harvard Medical School, was a member of the somatic symptoms disorders work group, and Robert S. Pynoos’73, professor in residence in psychiatry and biobehavioral sciences at UCLA, was a member of the anxiety, obsessive-compulsive spectrum, posttraumatic, and dissociative disorders work group.
The process of creating a new edition of the DSM, the first in almost two decades, stretched out over 13 years, including the first eight years that were focused on developing a research agenda. Once the work groups were formed in 2007, their members, drawn from hospitals and universities across the United States and overseas, began the process by conducting comprehensive literature reviews as well as analyzing secondary data sets to determine what changes needed to be made. Based on this review, proposed changes to the diagnostic definitions were made and posted on a public website for comment and feedback.
Dr. Walsh’s work group colleague, Evelyn Attia, MD, professor of psychiatry and a 1986 graduate of P&S, says the group “saw our task as taking a careful look at how the definitions for the eating disorders were working, and if something was working well, to leave it be. But if we had enough data to indicate that a definition was not working well or did not correspond with the current literature on a disorder, we were going to use the data to make changes.”
Each work group then submitted its draft for both internal review and public comment—a process
Dr. Walsh calls “not complicated, but demanding. We had to provide written justification for any significant change we recommended,” he says. “Then the proposals would be reviewed by several committees, to ensure quality control and that the recommendations passed scientific rigor.”
‘It’s a matter of formulating more precise delineation, not of pathologizing normal behavior.’
The eating disorders section underwent significant revisions. A number of new disorders are listed, including binge eating disorder, whose sufferers have uncontrolled episodes of binge eating but unlike those with bulimia nervosa do not purge themselves afterward, and Avoidance Restrictive Food Intake Disorder (ARFID), a disorder involving an eating disturbance that results in very low weight or nutritional deficiency for reasons other than a fear of fatness, such as avoiding eating solid foods after almost choking to death on some meat. Other changes involved improving diagnostic practices among clinicians. Dr. Shaffer’s work group, for example, was concerned with how bipolar disorder was being overdiagnosed in adolescents and children. “It was being used very loosely,” says Dr. Shaffer, “for chronically moody kids who would frequently have severe temper outbursts. Some people thought that this was the childhood version of adult bipolar disorder and no prospective follow-up studies have shown that such children go on to develop bipolar disorder. The best predictor of bipolar disorder is a prolonged depression in adolescence. Severe tantrums in early childhood predict later anxiety and mood problems, and the optimal treatment for this has not been adequately studied. The bipolar label tended to limit treatment options. We wanted to address this problem in DSM-5 by adding a new disorder to cover such presentations, called disruptive mood dysregulation disorder, so that clinicians would have a proper diagnostic home for such children.”
For H. Blair Simpson, MD, PhD, professor of psychiatry at CUMC, who served on the anxiety work group, the biggest change involved the way several well-known anxiety disorders were categorized. “Some disorders that were included as part of the anxiety disorders section in DSM-IV have now been pulled out and placed into their own sections,” says Dr. Simpson. “In particular, posttraumatic stress disorder and obsessive-compulsive disorder are now each in their own chapters and grouped with different disorders.”
Another member of Dr. Simpson’s group, Roberto Lewis-Fernández, MD, professor of psychiatry at CUMC, focused on enhancing the cross-cultural validity of how disorders are described. The result was the “cultural formulation interview,” a guideline for clinicians to follow in evaluating the cultural aspects of patients’ symptoms.
“For example, a Hispanic person might come in and say he is seeing shadows or hearing his name called when he’s upset,” says Dr. Lewis-Fernández, who chaired a subgroup dealing with cultural issues. “In his culture, this is a common way of describing feeling distressed. But if the clinician doesn’t know that, he might mistakenly assume the person has a psychotic disorder. We wanted to clarify how that difference should be assessed, and I’m happy to say that DSM-5 has made several useful changes in that respect.”
DSM-5, like its predecessors, has attracted a good deal of controversy. By virtue of his position as APA president, Dr. Lieberman has become one of the manual’s main spokespersons. He is quick to respond to critics, both inside and outside the psychiatric profession, who assert that DSM-5 is guilty of “overdiagnosis,” labeling too many behaviors as disorders.
“That’s just plain wrong,” he says, adding that psychiatry is no different from other areas of medical science, which are constantly identifying diseases that were not previously recognized, such as autism (not distinctly identified until 1980) and hoarding disorder (now included in DSM-5). “It’s a matter of formulating more precise delineation, not of pathologizing normal behavior,” says Dr. Lieberman. “In fact DSM-5 actually has fewer diagnoses than DSM-IV as a result of consolidating some conditions like substance abuse and substance dependence disorders into substance use disorders.”
Another criticism is that DSM-5 does not reflect recent developments in neuroscience, biology, and genetics that have enhanced scientists’ understanding of the workings of the brain. But Dr. Lieberman believes the available research findings did not justify a wholesale reworking of the diagnostic nosology. “The architects of DSM-5, and psychiatry in general, would have liked nothing better than scientific advances to bring us to the point where we know that this gene or toxic protein or trauma produces this disorder, and you can make the diagnosis by a blood test or X-ray or the proper procedure,” he says. “God willing, that day will be coming very soon. But the reality is that we’re not there yet.”
Ultimately, despite these limitations in psychiatry’s understanding of the brain and the underlying causes of mental disorders, DSM-5 continues to be a vital tool for mental health professionals. “DSM-5 is an aid to help clinicians talk to other clinicians,” says Dr. Simpson. “Let’s say a clinician in Houston is treating someone with OCD (obsessive-compulsive disorder). When that patient moves to Seattle and the clinician wants to refer him, she can call up a doctor in Seattle and say, ‘This patient has OCD’ and describe the symptoms. Thanks to DSM-5, they are both using the same language for the clinical syndrome; they both know what they’re talking about.”
Other P&S psychiatry faculty also contributed to DSM-5. Michael B. First MD, professor and editor of DSM-IV-TR, a text revision of 1994’s DSM-IV, was an editorial and coding consultant for DSM-5. Michael R. Phillips, MD, professor, was on the mood disorders work group. Richard B. Krueger, MD, associate professor, and Heino Meyer-Bahlburg, Dr. rer. nat., professor, were on the sexual and gender identity disorders work group. Deborah Hasin, PhD, professor of epidemiology (in psychiatry) at CUMC, was on the substance-related disorders work group.
- Log in to post comments